Psoriasis
Psoriasis is a common, chronic inflammatory condition, caused by dysfunction of the immune system, which results in skin cells reproducing at a faster rate than normal.1,2,3 As a result, raised patches form on the surface of the skin, which can appear red or purple and be flaky, itchy and scaly.2
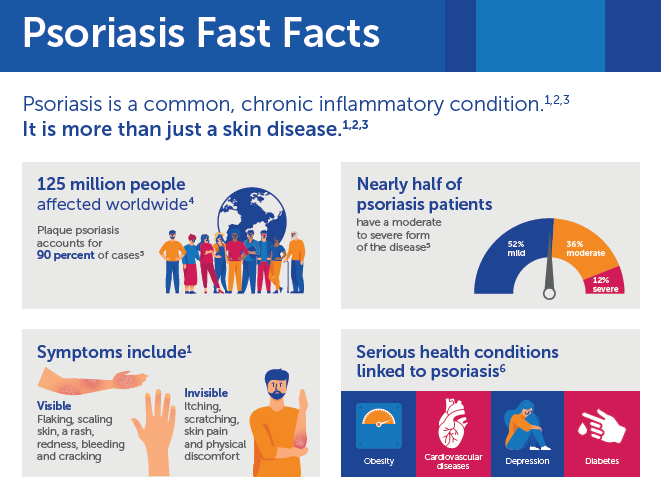
Psoriasis affects approximately 125 million people worldwide and is a life-long condition, for which there is no cure.2,3,4
Nearly half of psoriasis patients have a moderate to severe form of the disease.5
Women and men of all ages and ethnicities can be affected by psoriasis.1 There are many types of psoriasis, though plaque psoriasis is the most prevalent, comprising approximately 90 percent of all psoriasis cases.5
Several other serious health conditions have been associated with psoriasis, including diabetes, obesity, cardiovascular disease, depression, stroke and psoriatic arthritis – a chronic disease that causes inflammation, swelling and pain in the joints.1,6
Impact
Because of its visible and physically debilitating impact, psoriasis often takes an emotional toll on those who have it.7 The specific location in which symptoms appear on the body has been shown to have a direct link to the impact of psoriasis on patients’ quality of life, as visible psoriasis in noticeable areas, such as the scalp, nails and hands can be highly stigmatizing.8,9,10
People with psoriasis have experienced feelings of stigmatization, shame, embarrassment, anger or worry because of their condition.11,12
People living with psoriasis also frequently report sleeping problems, difficulties at work, issues interacting with family members, disrupted leisure activities and sexual difficulties.13,14 They also report that the significant impact the disease has on their quality of life is not well understood by physicians.15
Symptoms
Symptoms of psoriasis can vary from person to person. People with psoriasis may have symptoms of flaking, scaling, itching and scratching, a rash, skin pain, bleeding, redness, skin drying and cracking, and physical discomfort.16
Psoriasis can flare up anywhere on the body and can be severe or mild.2 Symptoms occur most often on the lower back, knees, elbows, legs, soles of the feet, scalp, face and palms but can also affect the hands, nails, skin folds and genital area.3,17
Types
The form of psoriasis with the highest prevalence is plaque psoriasis,5 which causes dry, raised, red skin lesions (plaques) covered with silvery scales.3 The plaques may be itchy or painful and can occur anywhere on the body, including the scalp, knees, elbows and lower back.3
- Nail psoriasis – Can cause fingernails and toenails to become pitted, discoloured or to grow abnormally.3 Psoriatic nails may become loose and separate from the nail bed (onycholysis), which in severe cases may cause the nail to crumble.3
- Guttate psoriasis – Primarily affects young adults and children and is regularly triggered by a bacterial infection.3
- Inverse psoriasis – Mainly affects the skin in the folds of the groin, breasts and buttocks, and may be triggered by fungal infections.3
- Pustular psoriasis – Can occur in widespread patches or in smaller areas on the hands or feet, causing pus-filled lesions.3
- Erythrodermic psoriasis – The least common type of psoriasis, can cover the entire body with a red, peeling rash that can itch or burn intensely.3
Causes and risk factors
While it isn’t entirely clear exactly what causes the immune system to malfunction in people with psoriasis, researchers have discovered genes that are linked to the development of the condition, and it is believed that environmental factors also play a role.18 There are a number of key factors which contribute to the onset and exacerbation of psoriasis, including:19
Genetics
Studies have shown a positive family history in approximately 35 percent of people with psoriasis.19
Medications
Numerous medications can trigger psoriasis, including lithium, nonsteroidal anti-inflammatory drugs, antimalarials, beta-blockers and angiotensin-converting enzyme inhibitors.19
Infection
Streptococcus, HIV, fungi and other bacterial and viral infections have been found to trigger or exacerbate psoriasis.19
Lifestyle
Obesity, smoking and stress are factors which are thought to increase the risk of psoriasis.3,19

Management
In the past 15 years, breakthroughs in the understanding of how psoriasis develops have resulted in the advancement of targeted and highly effective therapies.20 However, unmet needs remain in the treatment of psoriasis; a population-based survey identified that approximately one in three psoriasis patients reported that their primary goals of therapy, including keeping symptoms under control, reducing itching and decreasing flaking, were not met with their current treatment.21
For people with mild psoriasis, topical agents remain the mainstay of treatment.22 Moderate to severe plaque psoriasis should be treated systemically, and in many countries biologics are recommended as an option for first-line treatment.22
As clinical studies continue to demonstrate the serious, systemic effects of psoriasis, new research approaches are needed to support our understanding of effective treatment options and ultimately improve the health and lives of people with psoriasis.20